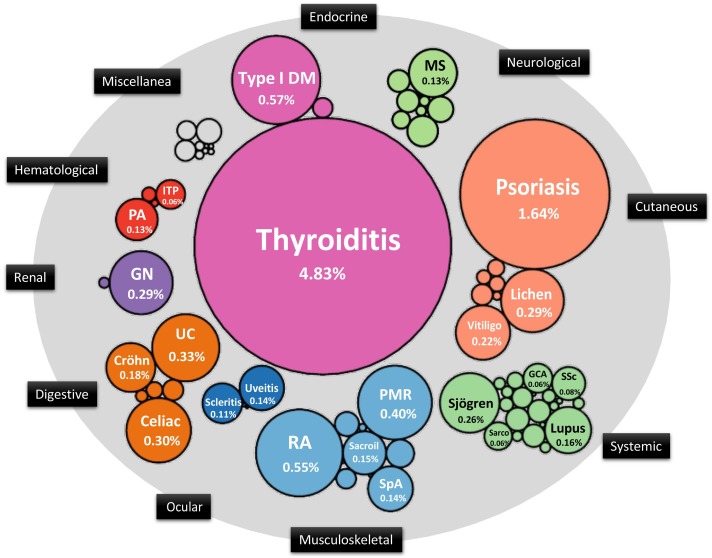
An autoimmune condition arises when the immune system is unable to differentiate between healthy tissue/cells and potentially harmful antigens (invaders). A study in Catalonia, Spain during the period 2012-2017 found that >10% of the population had an autoimmune diagnosis (1) with 78 different autoimmune conditions identified (Fig 1), with women being twice as likely to have a diagnosis. There are more than 100 different autoimmune conditions, each has its own symptoms, age of onset and overall effect on the diagnosed individual.
Autoimmune conditions fall into one of two categories: organ-specific (eg Hashimoto’s Thyroiditis) and systemic (eg. Lupus). They often take many years to develop and be diagnosed, and when they are, the individual may feel devastated, confused and yet relieved that finally, they know what’s going on. There are multiple factors that drive the development of autoimmunity: genetic predisposition, the microbiome, barrier integrity and environmental triggers. The latter include diet, stress, exposure to toxins, sunlight exposure, infections, and lifestyle choices such as smoking and exercise.
Autoimmune conditions are frequently associated with increased intestinal permeability (often described as Leaky Gut) in which particles of partially digested food and other molecules are able to pass through the gut wall into the bloodstream (2). Here, the immune system identifies these particles as “invaders” (foreign bodies) and attacks them. These particles often have a similar structure to healthy tissue, and this is how the immune system may mistake healthy tissue for the “invader”, a process known as molecular mimicry. The body is particularly vulnerable to this when the immune system is under strain dealing with other demands such as stress or infection. Part of the immune system’s role is to remember previous “invaders” and if molecular mimicry continues, attacks on healthy tissue may reoccur.
Gut microbiome imbalance (dysbiosis) is well-documented in the pathogenesis of autoimmune conditions. Future host-microbiome studies will further clarify the mechanisms underlying how microbiome imbalance affects the disease progression (3). However, we can promote a healthy microbiome through our diet and lifestyle choices (4,5), thus supporting a healthy immune system, 70% of which resides in the gut.
An autoimmune condition presenting with accompanying gastrointestinal issues or one that is associated with celiac disease, investigation into celiac disease associated autoantibodies should be undertaken (6). Gluten, found in grains, is a well-established irritant to the gut triggering intestinal permeability and subsequent immune response (2). Gluten is also known to promote imbalance in the gut microbiome even in the absence of celiac disease (7). There is substantial evidence showing that gluten withdrawal may slow down the development of a non-celiac autoimmune condition. However, current knowledge has not yet established the mechanism underlying the beneficial effects of a gluten-free diet.
Working with a nutritional therapist can help identify foods and lifestyle adjustments, based on scientific evidence, that may help to manage an autoimmune condition, leading to an improved quality of life.
To find out more, please get in touch for a FREE no-obligation chat.
References
- Sisó-Almirall A, Kostov B, Martínez-Carbonell E, Brito-Zerón P, Ramirez PB, Acar-Denizli N, et al. The prevalence of 78 autoimmune diseases in Catalonia (MASCAT-PADRIS Big Data Project). Autoimmun Rev [Internet]. 2020 Feb 1 [cited 2020 Nov 17];19(2):102448. Available from: https://doi.org/10.1016/j.autrev.2019.102448 (Image taken from
- Fasano A. Leaky gut and autoimmune diseases. Clin Rev Allergy Immunol. 2012 [cited 2020 Nov 17]; 42(1):71–8. Available from: https://www.researchgate.net/profile/Alessio_Fasano/publication/51823457_Leaky_Gut_and_Autoimmune_Diseases/links/0046352cae0af3b5df000000/Leaky-Gut-and-Autoimmune-Diseases.pdf
- Khan MF, Wang H. Environmental Exposures and Autoimmune Diseases: Contribution of Gut Microbiome. Front Immunol [Internet]. 2020 Jan 10 [cited 2020 Nov 20];10:3094. Available from: https://doi.org/10.3389/fimmu.2019.03094
- Gershteyn IM, Burov AA, Miao BY, Morais VH, Ferreira LMR. Immunodietica: interrogating the role of diet in autoimmune disease. Int Immunol [Internet]. 2020 Aug 18 [cited 2020 Nov 17]; Available from: https://doi.org/10.1101/2020.05.05.079418
- Venter C, Eyerich S, Sarin T, Klatt KC. Nutrition and the immune system: A complicated tango [Internet]. Vol. 12, Nutrients. MDPI AG; 2020 [cited 2020 Nov 17]. p. 818. Available from: https://www.mdpi.com/2072-6643/12/3/818
- Lerner A, Ramesh A, Matthias T. Going gluten free in non-celiac autoimmune diseases: the missing ingredient. Expert Rev Clin Immunol [Internet]. 2018 Nov 2 [cited 2020 Nov 20];14(11):873–5. Available from: https://doi.org/10.1080/1744666X.2018.1524757
- Caio G, Lungaro L, Segata N, Guarino M, Zoli G, Volta U, et al. Effect of gluten-free diet on gut microbiota composition in patients with celiac disease and non-celiac gluten/wheat sensitivity. Nutrients. 2020 Jun 1;12(6):1–23.

